Appendicitis is defined as an inflammation of the inner lining of the
vermiform appendix that spreads to its other parts. This condition is a
common and urgent surgical illness with protean manifestations, generous
overlap with other clinical syndromes, and significant morbidity, which
increases with diagnostic delay (see Clinical Presentation). In fact,
despite diagnostic and therapeutic advancement in medicine, appendicitis
remains a clinical emergency and is one of the more common causes of
acute abdominal pain.
Signs and symptoms
Pain first, vomiting next and fever last has been described as the
classic presentation of acute appendicitis. Pain starts mid-abdomen, and
except in children below 3 years, tends to localize in the right iliac fossa
in a few hours. This pain can be elicited through various signs and can
be severe. Signs include localized findings in the right iliac fossa.
The abdominal wall becomes very sensitive to gentle pressure (palpation). Also, there is severe pain on sudden release of deep pressure in the lower abdomen (rebound tenderness).
In case of a retrocecal appendix, however, even deep pressure in the
right lower quadrant may fail to elicit tenderness (silent appendix),
the reason being that the cecum,
distended with gas, prevents the pressure exerted by the palpating hand
from reaching the inflamed appendix. Similarly, if the appendix lies
entirely within the pelvis, there is usually complete absence of
abdominal rigidity. In such cases, a digital rectal examination elicits tenderness in the rectovesical pouch. Coughing causes point tenderness in this area (McBurney's point)
and this is the least painful way to localize the inflamed appendix. If
the abdomen on palpation is also involuntarily guarded (rigid), there
should be a strong suspicion of peritonitis, requiring urgent surgical intervention.
Pain is not typical in some people, who may only have lower right
abdominal pain, and no mid-upper abdominal pain at the beginning. Often,
the pain is not prominent in the elderly or children below 3 years old.
Or the pain point moves to other locations, especially just below the
liver in a pregnant woman. In this case, the inflamed appendix is pushed
up by the enlarged uterus.[5]
Rovsing's sign
Continuous deep palpation starting from the left iliac fossa upwards (counterclockwise along the colon) may cause pain in the right iliac fossa, by pushing bowel contents towards the ileocaecal valve and thus increasing pressure around the appendix. This is the Rovsing's sign.[6]
Psoas sign
Main article: Psoas sign
Psoas sign or "Obraztsova's sign" is right lower-quadrant pain that
is produced with either the passive extension of the patient's right hip
(patient lying on left side, with knee in flexion) or by the patient's
active flexion of the right hip while supine. The pain elicited is due
to inflammation of the peritoneum overlying the iliopsoas muscles and
inflammation of the psoas muscles themselves. Straightening out the leg
causes pain because it stretches these muscles, while flexing the hip
activates the iliopsoas and therefore also causes pain.
Obturator sign
If an inflamed appendix is in contact with the obturator internus, spasm of the muscle can be demonstrated by flexing and internal rotation of the hip. This maneuver will cause pain in the hypogastrium.
Dunphy's sign
Increased pain in the right lower quadrant with coughing.[7]
Kocher's (Kosher's) sign
From the history given, the appearance of pain in the epigastric
region or around the stomach at the beginning of disease with a
subsequent shift to the right iliac region.
Sitkovskiy (Rosenstein)'s sign
Increased pain in the right iliac region as patient lies on his/her left side.
Bartomier-Michelson's sign
Increased pain on palpation at the right iliac region as patient lies
on his/her left side compared to when patient was on supine position.
[edit] Aure-Rozanova's sign
Increased pain on palpation with finger in right Petit triangle (can be a positive Shchetkin-Bloomberg's sign) - typical in retrocecal position of the appendix.[8]
Also referred as rebound tenderness. Deep palpation of the viscera over the suspected inflamed appendix followed by sudden release of the pressure causes the severe pain on the site indicating positive Blumberg's sign and peritonitis.[9]
Causes
On the basis of experimental evidence, acute appendicitis seems to be the end result of a primary obstruction of the appendix lumen (the inside space of a tubular structure).[10][11] Once this obstruction occurs, the appendix subsequently becomes filled with mucus and swells, increasing pressures within the lumen and the walls of the appendix, resulting in thrombosis and occlusion of the small vessels, and stasis of lymphatic flow. Rarely, spontaneous recovery can occur at this point. As the former progresses, the appendix becomes ischemic and then necrotic. As bacteria begin to leak out through the dying walls, pus
forms within and around the appendix (suppuration). The end result of
this cascade is appendiceal rupture (a 'burst appendix') causing peritonitis, which may lead to septicemia and eventually death.
The causative agents include foreign bodies, trauma, intestinal worms, lymphadenitis, and, most commonly, calcified fecal deposits known as appendicoliths or fecaliths[12] The occurrence of obstructing fecaliths
has attracted attention since their presence in patients with
appendicitis is significantly higher in developed than in developing
countries,[13] and an appendiceal fecalith is commonly associated with complicated appendicitis.[14]
Also, fecal stasis and arrest may play a role, as demonstrated by a
significantly lower number of bowel movements per week in patients with
acute appendicitis compared with healthy controls.[15]
The occurrence of a fecalith in the appendix seems to be attributed to a
right-sided fecal retention reservoir in the colon and a prolonged
transit time.[16]
From epidemiological data, it has been stated that diverticular disease
and adenomatous polyps were unknown and colon cancer exceedingly rare
in communities exempt for appendicitis.[17][18] Also, acute appendicitis has been shown to occur antecedent to cancer in the colon and rectum.[19] Several studies offer evidence that a low fiber intake is involved in the pathogenesis of appendicitis[20] .[21][22]
This is in accordance with the occurrence of a right-sided fecal
reservoir and the fact that dietary fiber reduces transit time.[23]
Diagnosis
Diagnosis is based on patient history (symptoms) and physical
examination backed by an elevation of neutrophilic white blood cells.
Histories fall into two categories, typical and atypical. Typical
appendicitis usually includes abdominal pain beginning in the region of
the umbilicus for several hours, associated with anorexia, nausea or
vomiting. The pain then "settles" into the right lower quadrant, where
tenderness develops. Atypical histories lack this typical progression
and may include pain in the right lower quadrant as an initial symptom.
Atypical histories often require imaging with ultrasound and/or CT
scanning.[24] A pregnancy test is vital in all women of child bearing age, as ectopic pregnancies
and appendicitis present similar symptoms. The consequences of missing
an ectopic pregnancy are serious, and potentially life threatening.
Furthermore the general principles of approaching abdominal pain in
women (in so much that it is different from the approach in men) should
be appreciated.
Blood test
Most patients suspected of having appendicitis would be asked to do a
blood test. Half of the time, the blood test is normal, so it is not
foolproof in diagnosing appendicitis.
Two forms of blood tests are commonly done: Full blood count (FBC),
also known as complete blood count (CBC), is an inexpensive and commonly
requested blood test. It involves measuring the blood for its richness
in red blood cells, as well as the number of the various white blood
cell constituents in it. The number of white cells in the blood is
usually less than 10,000 cells per cubic millimeter. An abnormal rise in
the number of white blood cells in the blood is a crude indicator of
infection or inflammation going on in the body. Such a rise is not
specific to appendicitis alone. If it is abnormally elevated, with a
good history and examination findings pointing towards appendicitis, the
likelihood of having the disease is higher. In pregnancy, elevation of
white blood cells may be normal, without any infection present.
C-reactive protein
(CRP) is an acute-phase response protein produced by the liver in
response to any infection or inflammatory process in the body. Again,
like the FBC, it is not a specific test. It is another crude marker of
infection or inflammation. Inflammation at ANY site can lead to a rise
in CRP. A significant rise in CRP, with corresponding signs and symptoms
of appendicitis, is a useful indicator in the diagnosis of
appendicitis. If the CRP continues to be normal after 72 hours of the
onset of pain, the appendicitis likely will resolve on its own without
intervention. A worsening CRP with good history is a sure signal of
impending perforation or rupture and abscess formation.
[edit] Urine test
A urine test in appendicitis is usually normal. It may, however, show
blood if the appendix is rubbing on the bladder, causing irritation. A
urine test or urinalysis is compulsory in women, to rule out pregnancy
in appendicitis, as well to help ensure that the abdominal pain felt and
thought to be acute appendicitis is not in fact, due to ectopic
pregnancy.
X–Ray
In 10% of patients with appendicitis, plain abdominal x-ray may
demonstrate hard formed feces in the lumen of the appendix (Fecolith).
It is agreed that the finding of Fecolith in the appendix on X – ray
alone is a reason to operate to remove the appendix, because of the
potential to cause worsening symptoms. In this respect, a plain
abdominal X-ray may be useful in the diagnosis of appendicitis, though
plain abdominal x- ray is no longer requested routinely in suspected
cases of appendicitis. An abdominal X – ray may be done with a barium
enema contrast to diagnose appendicitis. Barium enema is whitish fluid
that is passed up into the rectum to act as a contrast. It will usually
fill the whole of the large bowel. In normal appendix, the lumen will be
present and the barium fills it up and is seen when the x-ray film is
shot. In appendicitis, the lumen of the appendix will not be visible on
the barium film.
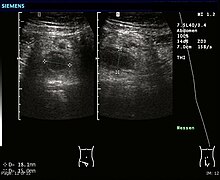
Ultrasound
Ultrasonography and Doppler sonography
provide useful means to detect appendicitis, especially in children,
and shows free fluid collection in the right iliac fossa, along with a
visible appendix without blood flow in color Doppler. In some cases (15%
approximately), however, ultrasonography of the iliac fossa
does not reveal any abnormalities despite the presence of appendicitis.
This is especially true of early appendicitis before the appendix has
become significantly distended and in adults where larger amounts of fat
and bowel gas make actually seeing the appendix technically difficult.
Despite these limitations, sonographic imaging in experienced hands can
often distinguish between appendicitis and other diseases with very
similar symptoms, such as inflammation of lymph nodes near the appendix or pain originating from other pelvic organs such as the ovaries or fallopian tubes.
Computed tomography
Where it is readily available, CT scan
has become frequently used, especially in adults whose diagnosis is not
obvious on history and physical examination. Concerns about radiation,
however, tend to limit use of CT in pregnant women and children. A
properly performed CT scan with modern equipment has a detection rate
(sensitivity) of over 95%, and a similar specificity.
Signs of appendicitis on CT scan include lack of oral contrast (oral
dye) in the appendix, direct visualization of appendiceal enlargement
(greater than 6 mm in cross-sectional diameter), and appendiceal wall
enhancement with IV contrast (IV dye). The inflammation caused by
appendicitis in the surrounding peritoneal fat (so called "fat
stranding") can also be observed on CT, providing a mechanism to detect
early appendicitis and a clue that appendicitis may be present even when
the appendix is not well seen. Thus, diagnosis of appendicitis by CT is
made more difficult in very thin patients and in children, both of whom
tend to lack significant fat within the abdomen. The utility of CT
scanning is made clear, however, by the impact it has had on negative
appendectomy rates. For example, use of CT for diagnosis of appendicitis
in Boston, MA has decreased the chance of finding a normal appendix at
surgery from 20% in the pre-CT era to only 3% according to data from the
Massachusetts General Hospital.
Ultrasound and CT compared
According to a systematic review from UC-San Francisco comparing
ultrasound vs. CT scan, CT scan is more accurate than ultrasound for the
diagnosis of appendicitis in adults and adolescents. CT scan has a sensitivity of 94%, specificity
of 95%, a positive likelihood ratio of 13.3 (CI, 9.9 to 17.9), and a
negative likelihood ratio of 0.09 (CI, 0.07 to 0.12). Ultrasonography
had an overall sensitivity of 86%, a specificity of 81%, a positive likelihood ratio of 5.8 (CI, 3.5 to 9.5), and a negative likelihood ratio of 0.19 (CI, 0.13 to 0.27).[25]
[edit] Alvarado score
| Migratory right iliac fossa pain | 1 point |
| Anorexia | 1 point |
| Nausea and vomiting | 1 point |
| Right iliac fossa tenderness | 2 points |
| Rebound tenderness | 1 point |
| Fever | 1 point |
| Leukocytosis | 2 points |
| Shift to left (segmented neutrophils) | 1 point |
| Total score | 10 points |
|---|
A number of clinical and laboratory-based scoring systems have been devised to assist diagnosis. The most widely used is Alvarado score. A score below 5 is strongly against a diagnosis of appendicitis,[26]
while a score of 7 or more is strongly predictive of acute
appendicitis. In patients with an equivocal score of 5 or 6, a CT scan
is used to further reduce the rate of negative appendicectomy.
Other data
- Tzanakis scoring
- Tzanakis and colleagues, in 2005 published a simplified system, now
called the Tzanakis scoring system for appendicitis, to aid the
diagnosis of appendicitis. It incorporates the presence of four
variables made up of specific signs and symptoms (presence of right
lower abdominal tenderness = 4 points and rebound tenderness = 3),
laboratory findings (presence of white blood cells greater than 12,000
in the blood = 2), as well as ultrasound findings (presence of positive
ultrasound scan findings of appendicitis = 6), to which scores are
allocated, in the computing of a scoring to predict the presence of
appendicitis.
The maximum score is a total score of 15; where a patient scores 8 or more points, there is greater than 96% chance that appendicitis exists.
Pathologic diagnosis
The definitive diagnosis is based on pathology. The histologic findings of appendicits are neutrophils in the muscularis propria.
Periappendicits, inflammation of tissues around the appendix, is often found in conjunction with other abdominal pathology.[27]
Differential diagnosis
- In children
- Gastroenteritis, mesenteric adenitis, Meckel's diverticulitis, intussusception, Henoch-Schönlein purpura, lobar pneumonia, urinary tract infection (abdominal pain in the absence of other symptoms can occur in children with UTI), new-onset Crohn's disease or ulcerative colitis, pancreatitis, and abdominal trauma from child abuse; distal intestinal obstruction syndrome in children with cystic fibrosis; typhlitis in children with leukemia;
- In women
- menarche, dysmenorrhea, severe menstrual cramps, Mittelschmerz, pelvic inflammatory disease, ectopic pregnancy
- In adults
- regional enteritis, renal colic, perforated peptic ulcer, pancreatitis, rectus sheath hematoma; in men: testicular torsion, new-onset Crohn's disease or ulcerative colitis; in women: pelvic inflammatory disease, ectopic pregnancy, endometriosis, torsion/rupture of ovarian cyst, Mittelschmerz (the passing of an egg in the ovaries approximately two weeks before an expected menstruation cycle)
- In elderly
- diverticulitis, intestinal obstruction, colonic carcinoma, mesenteric ischemia, leaking aortic aneurysm.
Management
Largely surgical, any conservative management is done at the
threshold of operation theater as the acutely inflamed appendix is
liable to rupture during such treatment.
The treatment begins by keeping the patient from eating or drinking in preparation for surgery. An intravenous drip is used to hydrate the patient. Antibiotics given intravenously such as cefuroxime and metronidazole
may be administered early to help kill bacteria and thus reduce the
spread of infection in the abdomen and postoperative complications in
the abdomen or wound. Equivocal cases may become more difficult to
assess with antibiotic treatment and benefit from serial examinations.
If the stomach is empty (no food in the past six hours) general
anaesthesia is usually used. Otherwise, spinal anaesthesia may be used.
Once the decision to perform an appendectomy has been made, the
preparation procedure takes more or less one to two hours. Meanwhile,
the surgeon will explain the surgery procedure and will present the
risks that must be considered when performing an appendectomy. With all
surgeries there are certain risks that must be evaluated before
performing the procedures. However, the risks are different depending on
the state of the appendix. If the appendix has not ruptured, the
complication rate is only about 3% but if the appendix has ruptured, the
complication rate rises to almost 59%.[28] The most usual complications that can occur are pneumonia, hernia of the incision, thrombophlebitis, bleeding or adhesions.
Recent evidence indicates that a delay in obtaining surgery after
admission results in no measurable difference in patient outcomes [29]
The surgeon will also explain how long the recovery process should
take. Abdomen hair is usually removed in order to avoid complications
that may appear regarding the incision. In most of the cases patients
experience nausea or vomiting which requires specific medication before
surgery. Antibiotics along with pain medication may also be
administrated prior to appendectomies.
Pain management
Pain from appendicitis can be severe. Strong (i.e., narcotic) pain
medications are recommended for pain management prior to surgery.
Morphine is generally the standard of care in adults and children in the
treatment of pain from appendicitis prior to surgery.[citation needed]
In the past (and in some medical textbooks that are still published
today), it was commonly accepted among the majority of academic sources[weasel words]
that pain medication not be given until the surgeon has the chance to
evaluate the patient, so as to not "corrupt" the findings of the
physical examination. This line of practice, combined with the fact that
surgeons may sometimes take hours to come to evaluate the patient,
especially if he or she is in the middle of surgery or has to drive in
from home, often leads to a situation that is ethically questionable at
best.[citation needed]
More recently, due to better understanding of the importance of pain
control in patients, it has been shown that the physical examination is
actually not dramatically disturbed when pain medication is given prior
to medical evaluation. Individual hospitals and clinics have adapted to
this new approach of pain management of appendicitis by developing a
compromise of allowing the surgeon a maximum time to arrive for
evaluation, such as 20 to 30 minutes, before active pain management is
initiated. Many surgeons also advocate this new approach of providing
pain management immediately rather than only after surgical evaluation.
Surgery
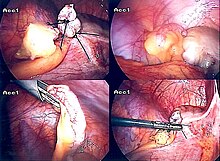
The surgical procedure for the removal of the appendix is called an appendicectomy (also known as an appendectomy). Often now the operation can be performed via a laparoscopic
approach, or via three small incisions with a camera to visualize the
area of interest in the abdomen. If the findings reveal suppurative
appendicitis with complications such as rupture, abscess, adhesions,
etc., conversion to open laparotomy may be necessary. An open laparotomy incision if required most often centers on the area of maximum tenderness, McBurney's point, in the right lower quadrant. A transverse or a gridiron diagonal incision is used most commonly.
According to a meta-analysis from the Cochrane Collaboration comparing laparoscopic
and open procedures, laparoscopic procedures seem to have various
advantages over the open procedure. Wound infections were less likely
after laparoscopic appendicectomy than after open appendicectomy (odds ratio (OR) 0.45; confidence interval
(CI) 0.35 to 0.58), but the incidence of intraabdominal abscesses was
increased (OR 2.48; CI 1.45 to 4.21). The duration of surgery was 12
minutes (CI 7 to 16) longer for laparoscopic procedures. Pain on day 1
after surgery was reduced after laparoscopic procedures by 9 mm (CI 5 to
13 mm) on a 100 millimeter visual analogue scale.
Hospital stay was shortened by 1.1 day (CI 0.6 to 1.5). Return to
normal activity, work, and sport occurred earlier after laparoscopic
procedures than after open procedures. While the operation costs of
laparoscopic procedures were significantly higher, the costs outside
hospital were reduced. Young female, obese, and employed patients seem
to benefit from the laparoscopic procedure more than other groups.[30]
There is debate whether emergency appendicectomy (within 6 hours of
admission) reduces the risk of perforation or complication versus urgent
appendicectomy (greater than 6 hours after admission). According to a
retrospective case review study [31]
no significant differences in perforation rate among the two groups
were noted (P=.397). Various complications (abscess formation,
re-admission) showed no significant differences (P=0.667, 0.999).
According to this study, beginning antibiotic therapy and delaying
appendicectomy from the middle of the night to the next day does not
significantly increase the risk of perforation or other complications.
This finding is important not simply for the convenience of the surgeons
and staff involved but for the fact that there have been other studies
that have shown that surgeries taking place during the night, when
people may be more tired and there are fewer staff available, have
higher rates of surgical complications.
Findings at the time of surgery are less severe in typical
appendicitis. With atypical histories, perforation is more common and
findings suggest perforation occurs at the beginning of symptoms. These
observations may fit a theory that acute (typical) appendicitis and
suppurative (atypical) appendicitis are two distinct disease processes.
(1)
Surgery may last from 30 minutes in typical appendicitis in thin patients to several hours in complicated cases.
Laparotomy explained
Laparotomy is the traditional type of surgery used for treating
appendicitis. This procedure consists in the removal of the infected
appendix through a single larger incision in the lower right area of the
abdomen.[32]
The incision in a laparotomy is usually 2-3 inches long. This type of
surgery is used also for visualizing and examining structures inside the
abdominal cavity and it is called exploratory laparotomy.
During a traditional appendectomy procedure, the patient is placed under general anesthesia
in order to keep his/her muscles completely relaxed and to keep the
patient unconscious. The incision is two to three inches (76 mm) long
and it is made in the right lower abdomen, several inches above the hip bone.[33] Once the incision opens the abdomen cavity and the appendix is identified, the surgeon
removes the infected tissue and cuts the appendix from the surrounding
tissue. After the surgeon inspects carefully and closely the infected
area and there are no signs that surrounding tissues are damaged or
infected, he will start closing the incision. This means sewing the
muscles and using surgical staples or stitches to close the skin up. In order to prevent infections the incision is covered with a sterile bandage. The entire procedure does not last longer than an hour if complications do not occur.
Laparoscopic surgery
The newer method to treat appendicitis is the laparoscopic surgery.
This surgical procedure consists of making three to four incisions in
the abdomen, each 0.25 to 0.5 inch (6.3 to 13 mm) long. This type of
appendectomy is made by inserting a special surgical tool called
laparoscope into one of the incisions. The laparoscope is connected to a
monitor outside the patient's body and it is designed to help the
surgeon to inspect the infected area in the abdomen. The other two
incisions are made for the specific removal of the appendix by using surgical instruments. Laparoscopic surgery also requires general anesthesia and it can last up to two hours. The latest methods are NOTES appendectomy pioneered in Coimbatore, India where there is no incision on the external skin[34] and SILS( Single incision laparoscopic Surgery)where a single 2.5 cm incision is made to perform the surgery.
After surgery
Hospital lengths of stay typically range from a few hours to a few
days, but can be a few weeks if complications occur. The recovery
process may vary depending on the severity of the condition, if the
appendix had ruptured or not before surgery. Appendix surgery recovery
is generally a lot faster if the appendix did not rupture.[35] It is important that patients respect their doctor's advice and limit their physical activity so the tissues can heal faster. Recovery after an appendectomy may not require diet changes or a lifestyle change.
After surgery occurs, the patient will be transferred to an postanesthesia care unit
so his or her vital signs can be closely monitored to detect
anesthesia- and/or surgery-related complications. Pain medication may
also be administered if necessary. After patients are completely awake,
they are moved into a hospital room to recover. Most individuals will be
offered clear liquids the day after the surgery, then progress to a
regular diet when the intestines start to function properly. Patients
are recommended to sit up on the edge of the bed and walk short
distances for several times a day. Moving is mandatory and pain
medication may be given if necessary. Full recovery from appendectomies
takes about four to six weeks, but can be prolonged to up to eight weeks
if the appendix had ruptured.
[edit] Prognosis
Most appendicitis patients recover easily with surgical treatment, but complications can occur if treatment is delayed or if peritonitis
occurs. Recovery time depends on age, condition, complications, and
other circumstances, including the amount of alcohol consumption, but
usually is between 10 and 28 days. For young children (around 10 years
old), the recovery takes three weeks.
The real possibility of life-threatening peritonitis is the reason
why acute appendicitis warrants speedy evaluation and treatment. The
patient may have to undergo a medical evacuation.
Appendectomies have occasionally been performed in emergency conditions
(i.e., outside of a proper hospital), when a timely medical evaluation
was impossible.
Typical acute appendicitis responds quickly to appendectomy and
occasionally will resolve spontaneously. If appendicitis resolves
spontaneously, it remains controversial whether an elective interval
appendectomy should be performed to prevent a recurrent episode of
appendicitis. Atypical appendicitis (associated with suppurative
appendicitis) is more difficult to diagnose and is more apt to be
complicated even when operated early. In either condition, prompt
diagnosis and appendectomy yield the best results with full recovery in
two to four weeks usually. Mortality and severe complications are
unusual but do occur, especially if peritonitis persists and is
untreated. Another entity known as appendicular lump is talked
about quite often. It happens when appendix is not removed early during
infection and omentum and intestine get adherent to it forming a
palpable lump. During this period, operation is risky unless there is
pus formation evident by fever and toxicity or by USG. Medical
management treats the condition.
An unusual complication of an appendectomy is "stump appendicitis":
inflammation occurs in the remnant appendiceal stump left after a prior
incomplete appendectomy.[36]







 – Mata sembab tentunya pernah dialami oleh sebagian besar orang. Dan
dengan mata sembab tentunya dapat mengganggu penampilan seseorang.
Biasanya, mata sembab diakibatkan karena seringnya begadang, sakit atau
diakibatkan oleh menangis yang lama. Namun mata sembab dapat dikurangi
maupun dihilangkan dengan langkah mudah. Berikut ini
– Mata sembab tentunya pernah dialami oleh sebagian besar orang. Dan
dengan mata sembab tentunya dapat mengganggu penampilan seseorang.
Biasanya, mata sembab diakibatkan karena seringnya begadang, sakit atau
diakibatkan oleh menangis yang lama. Namun mata sembab dapat dikurangi
maupun dihilangkan dengan langkah mudah. Berikut ini